This blog explores key facts every man should know about prostate health. The prostate gland plays a vital role in men’s health, particularly in reproductive and urinary function. As men age, the prostate is increasingly prone to conditions such as benign prostatic hyperplasia (BPH), prostatitis, and prostate cancer. Understanding how to maintain prostate health is essential for early detection, effective treatment, and long-term wellness.
What Is the Prostate and Why Is It Important?
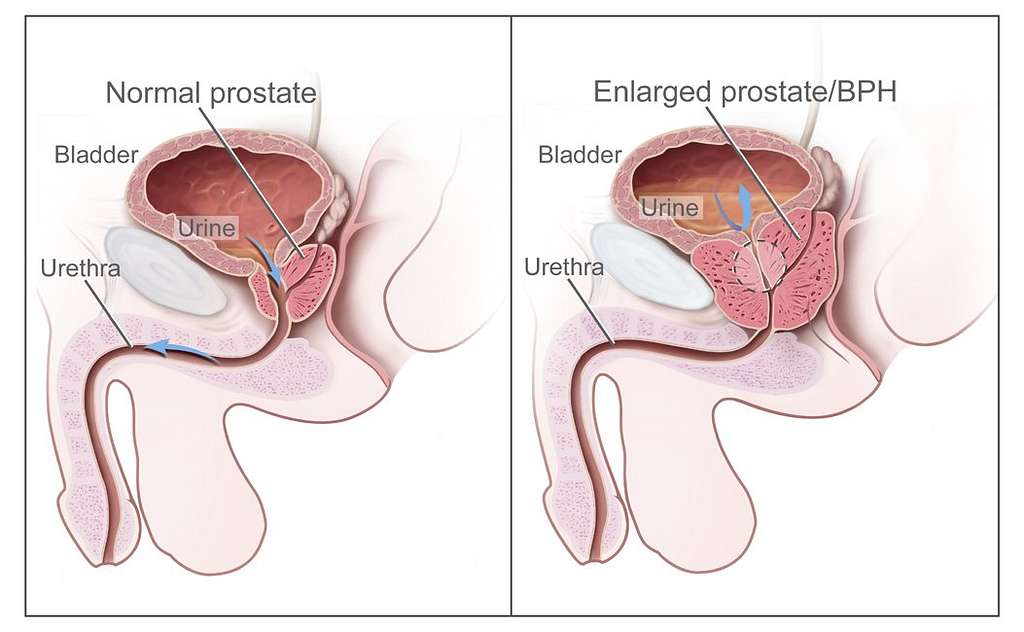
The prostate is a small gland, about the size of a walnut, located just below the bladder and in front of the rectum. It surrounds part of the urethra and produces seminal fluid, which helps nourish and transport sperm.
While its primary function is related to reproduction, the prostate also affects urinary function. As men age, changes in the prostate can lead to discomfort and complications, underscoring the importance of regular monitoring and preventive care.
Common Prostate Conditions
Several conditions commonly affect the prostate. Awareness of symptoms and early intervention can greatly improve outcomes.
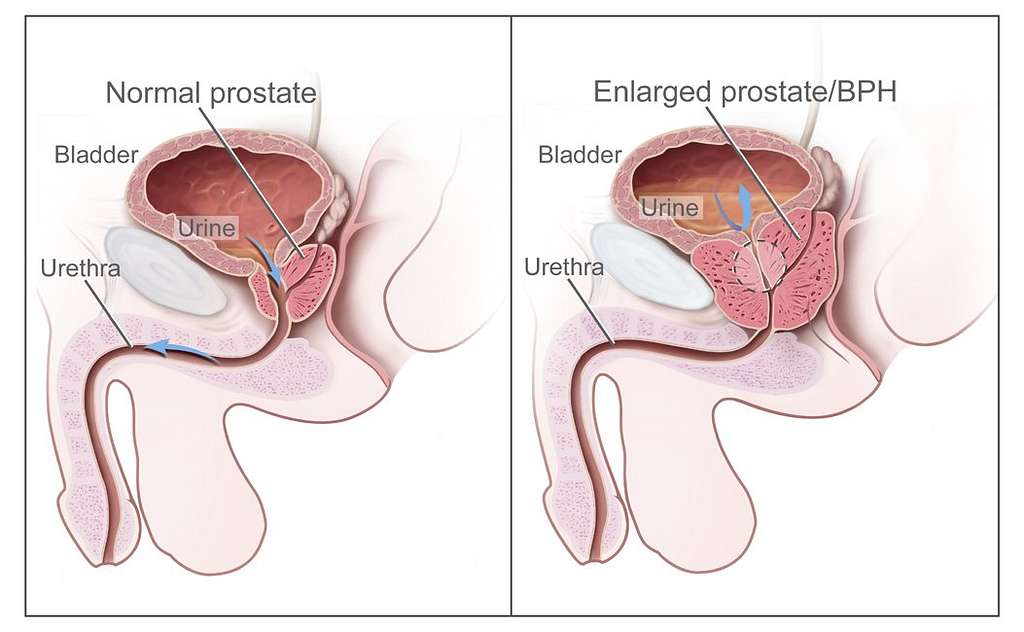
Benign Prostatic Hyperplasia (BPH)
BPH is a non-cancerous enlargement of the prostate gland that can obstruct urine flow.
- Frequent or urgent need to urinate
- Difficulty starting urination
- Weak urine stream or dribbling
- Incomplete emptying of the bladder
Treatments for BPH range from lifestyle changes and medications to minimally invasive procedures.
Prostatitis
Prostatitis is inflammation of the prostate, often caused by bacterial infection. It can be acute or chronic and affects men of all ages.
- Pelvic or groin pain
- Painful urination or ejaculation
- Flu-like symptoms (in acute cases)
Antibiotics are commonly used for bacterial prostatitis, while chronic cases may require longer-term management.
Prostate Cancer
Prostate cancer is the second most common cancer among men in the United States. It often develops slowly and may not cause symptoms initially, making screening crucial.
- Trouble urinating
- Blood in urine or semen
- Erectile dysfunction
- Pain in the hips or back (in advanced stages)
Screening and Early Detection
Routine screening for prostate issues is key to early detection and effective treatment.
Prostate-Specific Antigen (PSA) Test
This blood test measures the level of PSA, a protein produced by the prostate. Elevated PSA levels may indicate BPH, prostatitis, or cancer. While not definitive on its own, PSA testing is an important tool when combined with other evaluations.
Digital Rectal Exam (DRE)
During a DRE, a physician manually checks the prostate for size, shape, and abnormalities. Though quick, this exam provides valuable information, particularly when done alongside PSA testing.
Tips for Maintaining Prostate Health
Taking care of your prostate involves adopting healthy lifestyle habits:
- Eat a balanced diet: Focus on fruits, vegetables, whole grains, and foods rich in antioxidants.
- Stay physically active: Regular exercise supports hormone balance and immune health.
- Limit red meat and high-fat dairy: These have been associated with increased prostate cancer risk.
- Avoid smoking and reduce alcohol consumption: Both can contribute to chronic inflammation.
- Schedule regular checkups: Talk to your doctor about screening starting at age 50—or earlier if you’re at higher risk.
The Importance of Prostate Health: Conclusion
Understanding and prioritizing prostate health is essential for every man, especially as he ages. By recognizing the signs of common prostate conditions, adopting a healthy lifestyle, and staying on top of regular screenings, men can take proactive steps to maintain long-term wellness.
For expert urological care and prostate health evaluations, schedule a consultation with Dr. Yaniv Larish at Fifth Avenue Urology. Dr. Larish offers compassionate, comprehensive care using advanced diagnostic tools and treatment options.
FIFTH AVENUE UROLOGY
Dr. Yaniv Larish
5 East 83rd Street
New York, NY 10028
Phone: 212-675-3186
Learn more about Dr. Larish and his expertise:
https://www.fifthavenueurology.com/about-dr-yaniv-larish/

 Dr. Larish is a urologist and surgeon treating women and men with a variety of urological conditions. His expertise is in treating complex kidney stones, enlarged prostates (BPH), incontinence, erectile dysfunction, infertility, and urological oncology (prostate, bladder, kidney, and adrenal cancers). He is an expert in general urology and is often consulted for second opinions.
Dr. Larish is a urologist and surgeon treating women and men with a variety of urological conditions. His expertise is in treating complex kidney stones, enlarged prostates (BPH), incontinence, erectile dysfunction, infertility, and urological oncology (prostate, bladder, kidney, and adrenal cancers). He is an expert in general urology and is often consulted for second opinions.




 When behavioral strategies are not enough, medical therapies can be highly effective in managing OAB symptoms.
When behavioral strategies are not enough, medical therapies can be highly effective in managing OAB symptoms.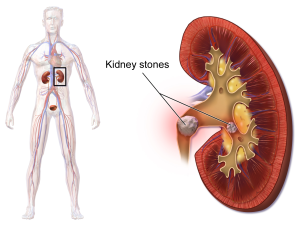

 This blog explores how to recognize the symptoms of urinary tract infections to highlight the significance of early diagnosis and treatment for a variety of urological issues. Urological health is an integral part of overall well-being for both men and women. Despite its importance, many people delay seeking treatment due to embarrassment or misconceptions about their symptoms.
This blog explores how to recognize the symptoms of urinary tract infections to highlight the significance of early diagnosis and treatment for a variety of urological issues. Urological health is an integral part of overall well-being for both men and women. Despite its importance, many people delay seeking treatment due to embarrassment or misconceptions about their symptoms.

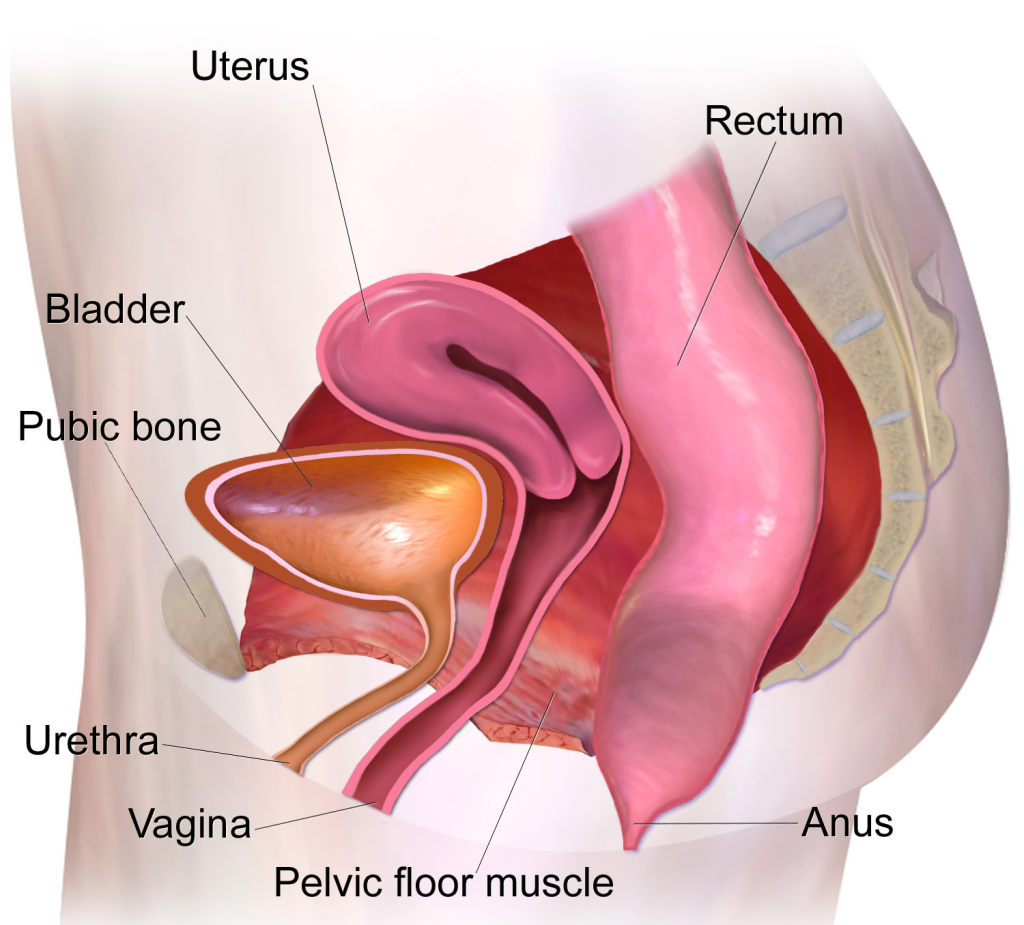
 Stress urinary incontinence (SUI) is a prevalent condition that affects many women, often leading to involuntary urine leakage during activities that put pressure on the bladder, such as coughing, sneezing, laughing, or exercising. If you’re living with SUI, you understand the impact it can have on your daily life and self-confidence. In this comprehensive guide, we’ll explore the causes, symptoms, and various treatment options available to help you regain control and improve your quality of life.
Stress urinary incontinence (SUI) is a prevalent condition that affects many women, often leading to involuntary urine leakage during activities that put pressure on the bladder, such as coughing, sneezing, laughing, or exercising. If you’re living with SUI, you understand the impact it can have on your daily life and self-confidence. In this comprehensive guide, we’ll explore the causes, symptoms, and various treatment options available to help you regain control and improve your quality of life. Several treatment options are available to address SUI in women. The choice of treatment depends on the severity of symptoms, the underlying causes, and individual preferences. Here are some common approaches:
Several treatment options are available to address SUI in women. The choice of treatment depends on the severity of symptoms, the underlying causes, and individual preferences. Here are some common approaches:
 If you’re considering treatment for stress urinary incontinence and are interested in the benefits of Solyx mini slings, it’s crucial to consult with a specialist.
If you’re considering treatment for stress urinary incontinence and are interested in the benefits of Solyx mini slings, it’s crucial to consult with a specialist. 